Adam Blatner
Words and Images from the Mind of Adam Blatner
The Humanities in Medicine
Originally posted on April 19, 2016
One of my roles is as an associate clinical professor of psychiatry at the local branch of Texas A&M Medical School, where I give occasional lectures on psychotherapy. Allied to that, I have an interest in supporting those who would promote the “Humanities in Medicine.”
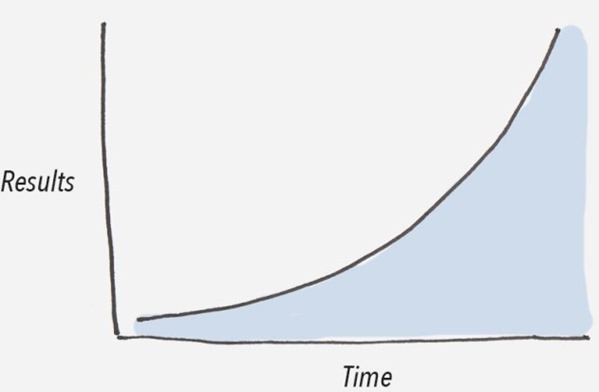
There’s a sore need for this, because most medical students suffer from an overload of information, along with the implication that they must know all the facts. Alas, these facts—or “differences that make a difference”—as the anthro-pologist and thinker Gregory Bateson called information—are now so plentiful as to be problematic. Using the analogy to the flow of water, the spring has become a trickle, a stream, a creek, a rivulet, a river, which then flows into a big river which then breaks up into a delta, and then a tsunami, a tidal wave as it operates as part of the sea. We have lived through much of this transition, which may be represented by an upwardly rising logarithmic curve! (This is the symbol for our time!)
It’s useful to have that concept articulated. Having words for it allows one to become more conscious of what’s happening in the world—of not only medical students, but all of us. The advances in our field are multiplying geometrically and it is really quite impossible to keep up. We are in the midst of this professional “explosion,” and our teaching institutions offer little to acknowledge this exponential amplification of what students are expected to know.
Meanwhile, the elementary skills and awareness of the plight of patients—I won’t dignify it by calling it “knowledge”—although some is, of course—offers a hint as to the evolution of the field at our doorstep. I recently read Pauline Chen’s 2008 book titled “Final Exam: A Surgeon’s Reflections on Mortality.” The author is a transplant surgeon. She talks of the need to integrate a bit of philosophy and even the new art of palliative medicine into the practice.
One solution is to empower patients to help you. Invite them to google around, participate in their own health care, dredge up information. Then work with their doctors to sift it, put it in perspective, and apply it.
There are so very many variables in patient care. “Disease” is merely an abstraction, a broad category. It has physical aspects and also dimensions of resistance that we know little about. Vitamin C plays a part. So does the mind. Psychology depends on such variables as ego strength, temperament, interests, family and cultural background, and other variables. So what we have is rather a person who exhibits elements of what we call disease or dysfunction, along with sub-types and nuances. In addition, I have no doubt that the morale (not morality) of patients, which reflect their experience in their social network, play a strong part. Similarly, patients’ broader function within their own historical era and culture, also generates a complex psychology, much deeper than psychoanalysis. I’m talking about the mysteries that have to do with healing, sickness, and dying.
Disease
A re-told history of medicine might be a welcome addition, as medical students seem blissfully embedded in a culture of overload, with oppressive elements, and shorn of context. For example, it may be that some diseases in the past have no present equivalent. Perhaps they were caused by a virus that has since disappeared or mutated significantly. For example, there are no fixed psychiatric diseases. We know of neurasthenia, common in the late 19th century, rarely if ever diagnosed today. Some so-called diseases were probably not diseases at all, but new diseases are cropping up, and one rarely hears about old diseases. For example, there were doctor-caused “iatrogenic” diseases such as childbed fever.
These were “caused” by a mixed development in medicine about 175-200 years ago. Starting in the late 18th century, there was the technology for examination of those who had died. The “autopsy”, was at the beginning of the 19th century a radical and enlightening teaching tool! Alas, bacteriology was unknown. So doctors washed their hands in a superficial fashion, and then, proud that they had learned things in new ways that previous generations of doctors had not, then failed to wash their hands thoroughly. They then proceeded to do rounds and do intra-vaginal “examinations” on women who gave birth, which gave them puerperal fever, a nasty and often fatal streptococcal and other germ infection of the uterus (or womb)! This is all the story of Ignaz Semmelweiss in Vienna, some 175 years ago in Europe! Do today’s medical students even know about such examples?
Thus, the Humanities in Medicine may help physicians and other healers to recognize all this. Healing operates in part at a deeper level that is not wholly individual-centered. It relates to social, and existential or faith integration. (Note that I am not promoting any particular world-view or religion.) All these are yet but still-germinating thoughts for further conversation and for my own contemplation.
Leave a Reply