Lecture 3: EARLY DEVELOPMENTS IN IMMUNIZATION
(Stories in the History of Medicine)
AdamBlatner, M.D.
February 9, 2009. Given as part of Senior University Georgetown's Winter-Spring, 2009 program.
Links to Lecture 1: Introduction, the Microscope, and the Beginnings of Germ Theory
Supplements to Lecture 1: A Very Brief Overview of the History of Medicine Ancient times to 1500
Overview 1500 - Present History of the Microscope
Lecture 2: Germ Theory: Pasteur, Lister and others. Lecture 4: The early history of anesthesia.
Lecture 5: Nutritional Deficiency Diseases Lecture 6: Prevention, sanitation, hookworm, dental plaque
Note on the terminology: Vaccination and immunization have become synonyms. Originally, however, the term "vaccination" applied only the process of immunization against smallpox, but then became generic for many other types of immunizations.
How Immunization Works
Hippocrates spoke about strengthening the body’s own resilient power, with good nutrition, exercise, sleep, good mental attitude. The nature of resilience is interesting, and it has to do with the physiological process called immunity. The reason germs don’t eat us up, rot us as if we were carrion, just dead tissue, is that we are constantly fighting off and neutralizing them. Right now in your body you may have a million incursions going on, viruses, bacteria, microscopic breaks in your body’s membranes, inner and outer, with tiny invasions, skirmishes, and ultimately, your body escalates until it defeats those invaders. It does this using literally hundreds of techniques, from white blood cells rushing to the part—and what we know as pus is really a mixture of fluid or mucus and dead bacteria and dead cells and especially lots of white blood cells—to a range of antibodies that attach to the germs and in various ways neutralize them or make them able to be eaten by certain white blood cells.
The process of inflammation itself is a marshaling of four ways the body uses to fight infection. The senses "foreign-ness" in the bacteria or virus, and nearby immune cells and injured cells release chemicals that:loosen the permeability of the little capillaries and more blood serum leaks into the surrounding, while the slightly larger arterioles enlarge—making the area red.
-- redness (Latin word: rubor) -- dilate the tiny arteries and capillaries, which then appear redder to the observer
-- warmth (calor) -- and the increased blood supply warms that part, and can be felt or measured
-- swelling (turgor) -- in the dilation or enlargement of the vessles, they become more permeable, allowing more serum and white cells to move out of the bloodstream into the surrounding tissues, making that area swell
-- pain (dolor)--- and the substances also irritate the pain receptors, making the organisms want to avoid stirring things up by moving; the immobility reduces the spread of the infection.
Observers since ancient time knew the signs, but not the causes---i.e., the billions of little large-protein-molecule foot-soldiers called antibodies that keep us protected. Those are the guys that get weakened in numbers by AIDS. Those are the guys who get brought forward to sustain us after we’ve already been infected by certain viruses and then we don’t get sick again.
Another process that gets activated when more than a tiny amount of infection happens is that the body senses this and increases the manufacture of white blood cells (which can be detected by doing a blood test or even finger-prick, counting the number of white cells and noting the percentage of each type). These cells migrate to the place of infection and when there are enough of them accumulating, it looks like pus. So that’s a brief review of the science here. The game is to provoke the manufacture of antibodies without having to subject us to the full impact of the more virulent form of the illness. Of course, people did this all the time—or their bodies did—or if the bodies didn’t enough, the people died— but human consciousness and purposeful intent wasn’t part of it. With this in mind, let’s look at the Time-Line and Subject we’ll address first.
Smallpox
We’ll start with one of the great plagues of humanity—especially since we became more urbanized, so probably it’s been around at least 6000 years. To the right is an electron microscopic photo, enlarged about 100,000 x.
Actually, the smallpox virus is relatively large, compared to most other viruses. Its effect is like a very muchmore severe form of chicken-pox. It can get in the eyes and cause blindness. And when the pustules heal, they leave a deeper scar, so it wrecks the complexion.
Smallpox in Ancient Times
Plagues have been mentioned in ancient texts. The Sumerian civilization thrived in what is now southeastern Iraq for over a thousand years (3200 - 2100 BCE) before the Assyrian Empire that is mentioned in the Bible (i.e., 900 - 600 BCE), and they wrote in a script that was made by wedges impressed on clay—so it was called “Cuneiform”
One of the texts that finally got deciphered around the time of many of the events given in this talk—that is, the later 19th century---was an epic story, the story ofGilgamesh, a sort of hero who sought immortality, with many sub-plots and diversions. One of those was a guy, Utna-Pishtim, who told a story that sounds a lot like the Great Flood of Noah—only it was part of the Middle East culture for more than a millennium before the Bible was written. Another story describes a big ol’ plague that well might have been smallpox.
In Egypt, evidence of the presence of smallpox is the markings on the face of the mummy of thePharaoah, Ramses V, around 1150 BCE:.
Baghdad
Staying in the Middle East, the next mention we'll make of smallpox is around 800 CE, in the then-flowering of Islamic culture. The Arabic scholars in their trade with the Byzantine Empire preserved many of the books of the ancients, such as those by Aristotle, Hippocrates, Galen, and others---since many of the originals were destroyed by the Crusaders in their attacks on Constantinople a few centuries later. This culture explored many sciences, and we get words like algebra and alchemy from the Arabic, the prefix "al-" meaning "the."
There were some important physicians in that culture, too, and one of them, Al-Rhazi---in Latin, "Rhazes,"---lived in Baghdad in that period. He wrote one of the earliest descriptions of the difference between smallpox and measles. Interestingly, at that time, smallpox in childhood was often milder. This is because when a disease is endemic—it is around a little all the time---then more people build immunity to varying degrees, as compared to diseases that are epidemic, that go away and don't come back for perhaps decades. The more endemic a disease, the more attenuated, the less virulent, the milder it becomes.
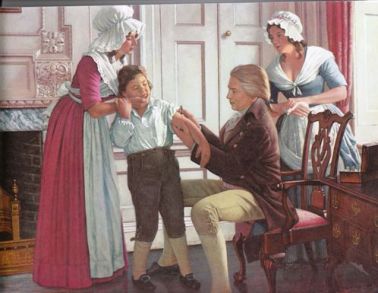
Here is Al-Rhazi examining a boy with smallpox.
The reason for the difference in severity has to do with the point of entry: If someone has the illness and they breathe out the viruses in their breath and you breathe in the droplets, it tends to get right into the deep system through the lungs, causes more fever, and then the blistering. Some folks die before the pocks even appear, from overwhelming system infection. Some people die from too many pustules, and some of those become secondarily infected with other germs and then general systemic infection with those germs, too. On the other hand, if your system has been exposed—we don’t yet know why—just a teeny bit, you pick up just enough immunity so that in some regions the infection was more like measles—it didn’t make you all that sicker than if you did get measles! This was true in the region around Baghdad in the early 800s CE.
I want to reinforce the idea that although much of world history taught in the mid 20th century was Eurocentric, it has become increasingly obvious that a great deal of wisdom and invention arose from cultures in Asia, such as paper, the concept of the zero, algebra, some ideas in medicine and chemistry, and so forth. I may have mentioned in earlier lectures that the era of flourishing of new ideas in the 14th through the 17th century called the Renaissance was fueled by the influx of written scholarly material from Ancient Greece preserved by the Arabic scholars, along with other types of trade with India and the Far East and elsewhere.
China
. Smallpox was present in China, and here's a picture of a Chinese god, Yuohoa Long, who was appealed to for healing of smallpox
And then around 900 CE, some Chinese physician wrote about the first preventive approach, called insufflation: if one blows a tiny bit of powdered scab from a healing smallpox patient into the nose of someone who hadn’t yet gotten the disease, they became slightly ill for a couple of days and then were immune.
Similarly, someone noticed that if you get a little smallpox through the skin, through the blankets of someone, say, it tends in most cases to cause a relatively mild case. If one is relatively what we would call nowadays immuno-suppressed for all sorts of reasons, anemia, malnutrition, who knows—maybe 10% of those inoculated would get a bigger reaction and 2% would die!
But if you don’t get inoculated, maybe 40% will get the disease, maybe more, and 14% will die, plus there are those who are literally blinded by the disease, and others’ faces are terribly pockmarked. So those were the odds as we shift into the next part of our story.
A little more about smallpox: In Latin this disease is called variola, and epidemics of it have swept the world since time immemorial. It’s not clear why, but in communities where it’s been around, it’s not as bad as in communities where it hasn’t been around at all. So in Europe in the 17th century or thereabouts, where smallpox had been around, some people died from the disease; some people were blinded by it; but most folks who got it did not die. Their skin would be deeply pock-marked, though, and it ruined your complexion. In the New World, the Americas, after Cortez landed, someone had smallpox and it ran through the central American indians like wildfire, killing the majority of people who caught it. It was the real reason Montezuma’s army wasn’t able to fight the Spaniards. It also killed significant percentages —often a majority—of north American Indian people, and again, made it possible for the “conquest” (by unintentional—usually—biological warfare) by the Europeans. We should not underestimate the trauma and demoralization, the deep shaking of the religious faith, of a people when a plague sweeps through and kills more than thirty per cent, and sometimes as high as seventy per cent of a population! The Black Plague transformed Europe and Smallpox, Measles, and Influenza among others did likewise to the North American Indians six or seven hundred years later.
Lady Mary Wortley Montagu
So the idea of inoculation was around in China, India, and drifted into Turkey, but physicians in Europe didn’t know about it, and epidemics of smallpox were not uncommon there for many centuries. All manner of kings and armies and dynasties were affected by deaths and epidemics.
Our first story begins with an aristocrat's daughter in England who was considered quite a beauty in her later teen years:. She , as she later was known, married—against her father’s will—but still married well. After she was married, taking the name of Lady Mary Wortley Montagu, she caught smallpox and recovered, but with many pock marks on her face. This was when she was around 22. She kept her adventurous spirit, though. Her husband was assigned as the ambassador to Constantinople around 1717 and she went. There she heard about inoculation and arranged to have her son inoculated. The story is more detailed and involved, but the son did well and she wrote to a friend in London about it. Later, after she returned to England with her husband, there was a daughter, and again she arranged for an inoculation. This time there were several doctors and observers and again it went well. The word spread, as did the practice.
Cotton Mather was a spokesman for inoculation. He had heard about it from a slave and was able to talk a local physician Dr. Boylston, to trying it out. This happened around 1721. It was both helpful and also controversial, and the good doctor at one point almost was lynched. Then the doctors took control and they introduced all sorts of what are now perceived as unnecessary provisions in order to lower the risk, including purging (i.e., giving substances that induce diarrhea), bleeding, special diets, etc. This was inconvenient and expensive. The method fell out of favor for a few decades in the mid-century, then re-emerged.
George Washington had his troops at Valley Forge variolated, inoculated with small amounts of smallpox through a scratch in the skin, because he did not want to risk his overall effort, fragile as it was, by having an epidemic lay his troops low.
Still, variolation, inoculation, was by no means a risk-free procedure.
Edward Jenner and Vaccination
As I mentioned, while inoculation was better, statistically, than nothing, if you caught it, especially from an inoculation, and you died from it, being statistically better didn’t count for much. Was there a way to get the same result with even less risk?It turns out there was, and it was discovered by Edward Jenner.
Jenner was a bright student and also amateur naturalist. He studied for a while with the well known John Hunter, who was at the time an eminent surgeon, anatomist, and character.
Jenner (right) noticed that milk- maids occasionally would pick up a kind of skin blister---i.e., cowpox---and the Latin term for that disease is vaccinia. This was a minor infection that was uncomfortable for a while, but never fatal. And they reported that they were then immune from smallpox. (Later, the principle here is that a light case of something gets the immune system up, and that something may be almost the same but not as bad as a similar germ-infection.)
It turns out that there were a few precursors, a farmer named Benjamin Jesty in 1774 had tried this. It seems that Jenner had not heard of this fellow. Anyway, in the early 1790s, Jenner did some experiments, developing the technique that came to be called vaccination, and finally tried it on a boy! The boy did okay, and had no reaction to a later inoculation.
Word of Jenner's vaccination method spread and became gradually more widely accepted. Above, right: Drawings of cowpox, from Jenner's classic 1798 paper about the method, and below those (upper right), an example of the lancet he used and other tools for this procedure.
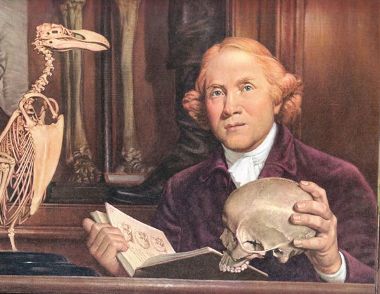
Benjamin Jesty, who inoculated his family with cowpox in 1774
Not that this story proceeded uneventfully. To the contrary! At one point in the story, Jenner's perhaps overly-generous expenditure of time and money promoting this new preventive device became problematical! He found himself (in modern dollars) around a million dollars in debt! Eventually he was able to get parliament to give him a grant that made up for much of his debt, and others also contributed, but the point was that the generosity and fairness of colleagues was not something that could be relied upon. Others claimed significant credit.
Another important point is that the method required a good deal of refining. One should not obtain the material from a cowpox that may have become secondarily infected with other germs, for example, and when then would be the best time and amount to take and then to inoculate?
So this builds on the problems that cropped up earlier in the century with variolation. As the method spread, though, there were many doubts and anti-vaccination responses. Here's a cartoon that shows people growing little cows from not only the vaccination site, but from their face, nose, and even growing horns under the hair. Oh, my!
There were movements to make smallpox mandatory, partly in response to another mini-epidemic in the early 19th century:
It worked, too, as shown in the illustration to the left. But there was also resistance to the method, and an active anti-vaccination movement was also operating. In this picture to the right below, a printed postal envelope carries the propaganda: On the back of the envelope are are the words noted:
Louis Pasteur (Later Years' Work on Immunology)
The next story begins in the 1870s with ol’ Louis Pasteur, whom we heard about in the last lecture. It might be interesting to note that at age 46 (in 1868) Pasteur suffered a significant stroke and thereafter a good deal of help in his career depended on his wife, Marie Laurent Pasteur! He had made progress in establishing a plausible germ theory, finally, and this supported efforts at antisepsis and later asepsis, which made modern surgery possible and elevated the surgeon in status from a step or two below the physician to in many cases a step above the family physician.
It begins with an episode of serendipity, which is a nice way of saying oops! Let’s see what we can do with this. There have been a goodly number of such episodes in the history of medicine. Many a mistake has led to something better, and Pasteur himself was known for the saying, “Chance favors the prepared mind.” Just as they asked this chemist---remember, he was not a physician—but by that time, recognized as a pioneer of biology—to help with another small epidemic—chicken cholera (1878). There are diseases of animals that don’t immediately affect humans, but since agriculture is big, such diseases have immense economic importance. Anyway, Pasteur was doing some research: Inject chickens. Note how many die. By mistake, injected some chickens with culture that had sat around for a couple of weeks. They got sick but didn’t die. They were put back with other chickens. Then, after a short vacation, Pasteur and his colleagues returned and re-commenced their experiments, making up fresh cultures of the disease. After injection, as anticipated, all died---except---not anticipated---some of them didn't, and it turned out that these were the chickens who were injected previously and only became sick but recovered. This was the turning point.
It occurred to Pasteur that an attenuated germ, whether by heat, chemical, age, or other factor, might not be as virulent, yet able to evoke a protective response rather than just infecting and killing the new host. (He may have also seen the connection of this idea with the by-then established method of vaccination.) So Pasteur considered this and sought to work out another type of vaccine, this time for another animal disease—anthrax. We’ve heard about it as a weapon of bio-terrorism, but really it’s more of an animal disease that some folks get—usually as a cutaneous ulcer—wool sorter’s disease. Anyway, it kills sheep.
Once again Pasteur set to work and came up with a vaccine which he tested in 1881.
Its effectiveness was dramatic and Pasteur's status grew tremendously. (He was astutein inviting reporters to the experiment.) All this, incidentally, happened in the decade after a serious stroke!
Rabies
Once again, Pasteur set to work, addressing another problem, rabies, also known as mad-dog disease or hydrophobia. He couldn’t find the active agent, but was able to replicate the disease in rabbits as well as dogs. Then he thought about how to attenuate the virus. To make a long story short, he found that the degree to which he dried a dead rabbit’s spinal cord—one that had rabies—the less virulent would be the effect. So this time, he tried a series of injections, beginning with the least virulent solution, and each following injection then having a slightly stronger or more virulent solution. He found it worked on animals.
Pasteur was wary about trying it on humans, but in 1885 got a call about a boy who had been badly bitten by a rabid dog—and folks thought this was pretty desperate. So Pasteur tried it, the immunization method. And it seemed to work. (Scientifically, we now know that some people who are said to have been bitten by a rabid dog don’t get sick anyway, so who knows, but the treatment has continued to be validated.)
So, Chicken cholera, anthrax, rabies... and meanwhile, Pasteur was also moving into the role of a general institute leader, with a number of students who worked for him, and these guys then came up with a variety of other types of immunization.
Robert Koch (1843-1910)
Here was another pioneering scientist in East Germany (Prussia) who has been considered a key person in the emergence of bacteriology, and a listing of all his advances could fill many pages. Robert Koch was a bit of a rival to Pasteur because of a number of things---the French-German rivalry (around the time of the Franco-Prussian war) being part of it; Pasteur's not having acknowledged Koch's seminal work with anthrax as a foundation for Pasteur's later development of the vaccine; and so forth. He was younger than Pasteur by 21 years, and was in his mid 40s when he was really getting going. Koch critiqued with some validity methodologic errors in Pasteur’s work. Truth be told, both these guys and everyone else had their own character flaws. Just because you’re excellent in one or several roles doesn’t mean you might not have other roles in which you’re mediocre or even problematic. Pasteur did tend to ignore others’ work. Anyway, Koch's work was substantial and he was given a Nobel Prize for it in 1905 in Physiology or Medicine.
Koch was an eminent bacteriologist who also made a foray into immunization. He did great work in finally culturing the bacterium of Tuberculosis—it’s very slow growing, that’s the problem— and then in the mid-1890s came up with a vaccine made out of killed bacteria in solution. It was not particularly effective, and the story was complex and a cautionary tale of what happens when social pressures to do something—this was at the height of the tuberculosis epidemic of sorts in Europe— were so great.
Behring and Passive Immunization (Anti-Toxins)
Emil Behring (on the right in the picture), later awarded a peer-status so that he could be called “von” Behring, worked in Koch's laboratory. He figured out the first approach to passive immunization. Let the horse or cow build the immune antibodies (they didn’t know what those were back then), to the toxin or germ, and then give the serum full of antibodies to the person who suffers. It works faster, targets only the person who gets sick.
Diphtheria
One of the greatest scourges of mankind was diphtheria. With outbreaks often reaching epidemic proportions, it killed about 50% of its victims, most of whom were children. Parents helplessly watched their children--unable to breathe due to closed-off air passages--die a horrible, black-faced death. Most of those who managed to survive were left with damaged hearts or paralyzed throats.
In America, diphtheria epidemics started to occur in 1735. In New England alone, the disease killed more than 5,000 children within five years. Worldwide, it took hundreds of thousands of lives during the next 150 years. As it happens, diphtheria became one of the first infectious illness to be conquered. Edwin Klebs and Friedrich Loeffler, German bacteriologists, discovered and isolated the bacillus that caused diphtheria. Then, the achievement of Pasteur—who five years earlier had administered the first protective vaccine for the treatment of rabies—was taken one step further: Emil von Behring, working at Koch's Institute for Infectious Disease, discovered the first therapeutic serum antitoxin in 1890. With his successful treatment of a child in 1891, Von Behring showed that the serum of animals that had been immunized against diphtheria could be used as a cure. It worked by neutralizing the toxin produced by the bacteria.
In 1894, von Behring began producing diphtheria antitoxin commercially, and the pharmaceutical and medical world would forever be changed. The Health Department in New York City was one of the first municipal authorities to use the antitoxin in 1894. Thereafter, the race was on to find other antitoxins and vaccines.
How these anti-toxins work: The gram-positive types of bacteria that cause botulism, diphtheria, and tetanus, among other diseases, give off a protein substance that is toxic to tissues and the heart or in other ways. Inoculations of animals with smaller, then larger doses, gradually evokes increasing levels of immune anti-toxin—we know now to be the toxin-protein-specific-antibodies. This is then withdrawn, concentrated, separated from blood cells, and bottled. Patients with tetanus or diphtheria, given this antitoxin, are helped to recover, or get past the hard parts. You may have heard of some stories of needing to fly an anti-toxin to some remote town in Alaska or some place, and this was the material.It should be noted that his co-worker in this endeavor was Shibasaburo Kitasato. (There were a number of advanced Japanese scientists participating in the medical frontier before the Second World War made it politically incorrect to acknowledge their activities!) In 1901 Behring won the first Nobel Prize for Medicine for his work on antitoxins.
Some recognition should be given also to Paul Erlich and others, who worked with Behring on these issues and went on to develop other aspects of immunology that go beyond the scope of this presentation. (Well, let's note that Erlich shared the 1908 Nobel Prize in Physiology or Medicine with Soviet biologist Elie Metchnikoff (1845-1916) for his work on immunity and serumtherapy.Other Immunological Developments
As time went on, people kept experimenting, learning more about other aspects of immunology---and these are innumerable and continue to expand! Active immunization substances were developed:
--1923, Diphtheria Vaccine --1926 Whooping Cough (Pertussis) Vaccine --1927 Tetanus Vaccine
--1927 Tuberculosis (BCG) Vaccine -- 1935 Yellow Fever Vaccine... then
-- 1955 Injectable Polio Vaccine (Salk) --1956, Oral Polio Vaccine (Sabin) -- 1964 Measles Vaccine
-- 1967 Mumps Vaccine 1970 Rubella vaccine (for German Measles)--- to prevent deafness or deformation in unborn fetuses
-- 1981 Hepatitis B -- 1981 Meningitis (meningococcus--improved in 2005) -- 1982, Pneumococcus Vacine
-- 1988, 1995, 2005, Improvements in Chicken Pox (varicella) vaccine
-- 1990 Hemophilus Influenza B (baby pneumonia) vaccine 1990 - Improvements in vaccines for Yellow Fever, Cholera, Typhoid Fever
-- 1993 Japanese Encephalitis
-- 1998, improved in 2003, Rota-Virus vaccine against gastro-intestinal flu of infancy and early childhood
-- 2001 Q Fever (Coxiella Burnetii, the most infectious disease in the world)
Of course, there could be stories for each of the following breatkthroughs, but I haven’t read up enough about the details.
The Conquest of Smallpox
To begin with where we started: A long, involved, politically complex story about how international agencies worked to clear up smallpox could be told here. Suffice it to say that efforts at immunization and vaccination have finally succeeded.
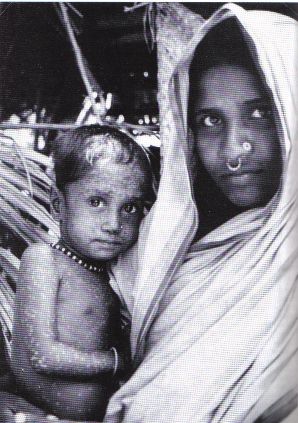
What may have been be one of the last cases of smallpox.
Polio immunization in India.