Some
diseases, like cholera, typhoid fever, and hookworm, may be prevented
by sanitary measures. Cholera and typhoid fever are linked to
contamination of food and water by the feces of those with those
diseases, from flies, impure water, not washing hands in food
preparation, and the like. Hookworm comes from walking barefoot near
feces infected with the worm's eggs, or otherwise letting skin connect
with moist ground. (This lecture also included a discussion of
dental hygiene, which is presented now as a separate webpage.)
Hygiene
"An ounce of prevention is worth a pound of
cure"--so goes an old proverb. Preventive approaches
in medicine have helped many more people
than all the medical
treatments ever given! My own career trajectory in the last decade has
been in the
direction of prevention, mainly through the vechicle of education, and
partly that through these lectures at
Senior University Georgetown.
Prevention has always been recognized as an important dimension in
medicine. The Greek god of healing, Aesculapius (right) had a daughter,
Hygeia (image at far right is a Roman statue dated around 100 CE), and
her hame then came to be applied to the general field of preventiive
health---i.e., "hygiene."
Previous lectures have addressed not only treatment, but also
prevention: Immunization and an understanding of the nature and
prevention of nutritional deficiencies are significant elements. This
lecture will be more related to sanitation. In dental hygiene, that
deals with brushing and flossing---to be presented in the
associated webpage.
This lecture will deal with two types of sanitation. Sanitation is an
euphemism, a nice way to say that we're dealing with feces---also
known, crudely, as "shit,"---a word that still seems a bit shocking.
This shock is in turn associated with a tendency to avoid that which is
disgusting. Freud made a point of noting that the avoidance of any
thoughts dealing with feces can be neurotic, especially when it
interferes with our thinking intelligently about how to dispose of our
waste products. In other words, because of this avoidance, there has
been a delay in
developing a rational, communal approach to sanitation, including the
provision of clean water, water treatment plants, well-built sewers,
fly control, and similar sanitary measures. Rose George recently wrote
an important book about how we deal with---and mostly avoid dealing
with---human feces; the book's title is
The Big Necessity (now at the Georgetown Library) see cover picture on left.
Cholera
The first disease to be mentioned has been around in Asia for
millennia, being described more fully in China in the 9th century, and
thereafter in the Middle East and India on several occasions. It hadn't
really spread into Europe and the West until around the early 19th
century, and then, for the next around 120 years, there were five or
six waves of epidemics with a surpiring degree of virulence and
rapidity of onset.
Cholera is a bacterial disease, and for the first two-thirds of the
century the germ theory itself was not established. Just as people can
catch a virus that invades and damages its cells, so too can bacteria,
though much smaller, also be invaded and affected by viruses! It turns
out that many of this general type of "vibrio" germ aren't so toxic,
but some are, especially when infected by a virus that feeds on it, and
makes it give off a toxin.
This toxin, in turn, blocks the
re-absorbtion of fluids from the intestine. In ordinary digestion, the
body secretes a great deal of fluid, which dissolves the nutrients
coming through, and almost all of this liquid and associated nutrients
are then reabsorbed. If you block this reabsorption, all the fluid remains in the
gut and the person develops a severe diarrhea, vomiting, and quite
rapidly, severe dehydration. The blood gets thicker and begins to block
up the arteries, oxygen can't get through, and the person often dies.
If you give the patient enough fluid and the right balance of
salts---because a lot of sodium, potassium and bicarbonate also is in
that intestinal liquid secretion---then they may recover, because the
body has a chance to mount an immune response. The key is getting that
fluid and the right balance of salts (i.e., "oral rehydration therapy") in right away.
Cholera was a frightening disease, and theories as to why it happened
were widespread. To the right below is a poster from a French magazine in the
mid-19th century.
|
I cannot express the depth of fear that comes with an
epidemic. The psychological consequences of living through several
waves of one or several types should be recognized as generating a
low-grade or more severe post-traumatic stress disorder—PTSD. There was a good deal of "blaming the victim," since
it often occurred in areas where poor people lived, and poor people
often were of a minority background. The political struggle was between
the private businesses and people of moderate wealth who, like today,
had reservations about their obligations to contribute to the common
good through developing the infrastructure. At that point---and often,
still today, in countries like India---it involves money to build
adequate sewer systems, water filtration and treatment plants, toilet
systems that kept the germs out of the drinking water,---and there were
legal actions taken to block community efforts at sanitation.
The trend of more people moving from the country to the city to find
work led to crowding, slums, and the city's lack of infra- structure
(e.g., sewers). I spoke about the filth of cities in the
second
lecture---the almost hopelessness about trying to ensure cleanliness
and the resultant spread of hospital based ("nosocomial") infections;
and the darkness of smog and child labor that made rickets common also
in the 19th century. As a result, an interesting movement happened in
medicine that was sort of right but for the wrong reasons: There were
many people who advocated what would be today thought of as intelligent
efforts at cleaning things up, sanitation, but this was because disease
didn't come from germs (so many thought then---hey, germs were just an
unproven "hypothesis" for most of the century!) but rather from miasma,
the toxic air that arose from unclean situations.
(Briefly, to review:
First Pandemic: 1817-1823, India, Middle East, etc.
Second: 1829-1849, India, Russia, in 1831, England, in 1832, the Americas,
– then again in England, Wales 1848
Third: 1852-1859, the most deadly, from India, devastated large swaths of
Asia, Europe, North America and Africa.
Fourth: 1863-1879, Bengal, Mecca, Europe, North America
Fifth: 1881-1896, India, Russia, Japan, Europe
Sixth: Asia, Africa through 1923 (a little less virulent, different strain bacterium
Seventh, on and off in underdeveloped countries.)
Contagionists versus Miasmatists
There were two schools of thought about cholera: One, that it was
caused by something noxious in the air, a miasma, associated with the
air coming up from the moist earth and rotting or fecal material. This
theory held sway during much of the previous 18th century and well into
the 19th century. The contagionists thought that disease was caused by
something that was catching, like smallpox or syphilis. Although it
turned out the contagionists were right about cholera, they didn't
understand the mode of contagion until halfway through the 19th
century; and although the miasmatists were wrong, technically---there
is no such thing as miasma, it turns out---their efforts at holistic
prevention and sanitation were more in the right direction in the long
run! This is one of the ironies and lessons of history! More about this
conflict as we go on.
|
Certainly things were fiilthy. Indeed, for a variety of ecological, economic,
technical, and political reasons, the 17th through the 19th century in
Europe became ever filthier. I should say by the words filth, or waste,
or fecal, all these are euphemisms for the earthier word—excuse
me—shit— and I say it for shock value, because that’s just the point:
People don’t want to be confronted by it, by the reminder that part of
their very real and necessary lives tends to be experienced as
disgusting. Freud himself noted that this area of awareness tends to be
repressed, taboo—and this essentially neurotic reaction has led to the
whole problem of waste disposal, fecal disposal be labeled
“sanitation”—again an euphemism—and one that far more often that is
wise tends to be marginalized, pushed off into the corner, swept under
the rug (ugh), and neglected until the complications of this neglect
come back to haunt us—and this is the social and historical lesson of
cholera.

|
Not that newspapers weren’t calling attention to the contamination
of the water: It was obviously polluted and full of bugs. The actual
shape and size of the bugs–the bacteria—wouldn’t be known for another
40-plus years, though—requiring an advance in the technologies of
microscopy and staining—we spoke about that in the first lecture.
In the earlier lectures on infection the main cause of disease was
mysterious and had many theories. One of the theories that gained a lot
of support was that there were “miasmas,” a word that refers to the
smelly air—it fits our intuitive perceptions that there’s something
wrong with the air, just as spoiled food tends to taste bad. And
as noted above, the stench of rotting garbage and open sewers was
powerful.
The contagionists spoke mainly about quarantine, and burning or
removing clothes, fumigating, isolating cases. In fact, for some
diseases, this in part worked. But the miasmatists felt the
contagionists neglected the miasma and the dirty conditions that caused
it. In fact, they turned out to be right, but for the wrong reasons. It
wasn’t the smelly air, it was the fecal contamination that goes with
flies and open sewers and other stuff that gets into the water.
Interestingly, you won’t get sick from fecal contamination, as
distasteful as that idea may seem—unless those feces contain germs or
worm eggs or some other disease—in which case you will catch that
disease. But there were a lot of those kinds of diseases—typhoid fever
and dysentery were very common and have a story that is more low-grade,
not so much epidemic as endemic—around a little all the time—but the
battle for sanitation is relevant to all of these.
Max von Pettenkofer
This Munich physician became established in an era when seeking
sanitation was already somewhat innovative. (This resonates with the
lesson of the
second lecture,
in which the students doing autopsies
were already enlightened compared to their parent's generation, so how
could enlightened people be mistaken?) Pettenkofer had become
well-known as a pioneer, and in terms of the actual effectiveness of
the work that needed to be done regarding creating an adequate sewage
system and water purifying plants, the "miasmatists" were perhaps even
more active than the "contagionists." Pettenkofer also wanted to
promote better nutrition, sunlight, adequate warmth in winter---indeed,
he was the kind of public-health minded holistic physician who
Dicken's character, Ebenezer Scrooge (in A Christmas Carol), would have
hated. Dr. Professor von Pettenkofer also had a good deal of status,
doing research in several fields such as biochemistry and physiology,
and in Munich would found a world-famous institute of
hygiene.
In addition, there had been pressure from pioneers such Edward
Chadwick—not a physician
but a civil servant—who fought consitently for several decades with the
entrenched interests in the
parliament. In the third corner there were those who, liked Scrooge,
only thought of themselves, and the poor could just fend for
themselves. They hired lawyers to argue for the rights of their clients
to pollute
as much as they want on their own property—a bit of libertarianism
versus the common good was a problem then as it is today!
So with all these edges, there needed to be a build-up of supporting
evidence. What’s wrong with
a little dirt, anyway? (Remember, this was a problem in the realm of
surgery and infections, all this happening in hospitals around the same
time!) Also, through the mid-19th century, no one had "seen" any
bacteria---or not so that it would be believed. (Actually, Leeuwenhoek
saw them over two centuries earlier!)
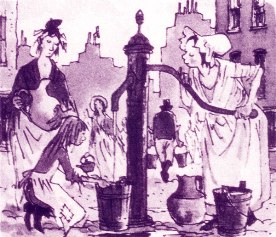
John Snow, M.D., and the Elucidation of the Cause of Cholera
Among the contagionists was .
Dr. John Snow(1813-1858).
(picture below), who has been generally credited for correctly
identifying the idea that leakage of contaminated water can carry
disease. Interestingly, we heard about Snow
a few lectures ago, in connection with his
being the one who used chloroform to alleviate the pain of childbirth
for Queen Victoria (Sadly, he
died unexpectedly from a stroke in 1858 at age 45, but his
epidemiological work on cholera continued to be vindicated. He's now
considered one of the earliest epidemiologists.) In the early 1840s, Snow studied the
problem and disagreed with the miasmatists, thinking that the disease
might be due instead to a kind of contagion---but not direct; rather,
through the water supply.
In
1848 Snow's researches into this subject was first published as a small
booklet,
On the mode of the
communication of cholera, and he kept accumulating evidence. A major breakthrough came
in a flare-up of cholera in London, in the Soho district. Snow
constructed one of the first "spot maps" for noting the distribution of
the deaths, and it became apparent that these centered on a water
supply, the Broad Street Pump. (That is, while Semmelweis assessed
numbers, Snow
assessed frequency and location.)
Snow first took the handle off the pump and noted a decline in the
incidence of the disease. Investigating further, Snow discovered that
there had been an old cesspool not far from the well that served the
pump! This was connected in turn to another cesspool in a house nearby,
and a child with cholera had had his diapers washed into that cesspool.
Further research on comparing the water supplies of different parts of
London confirmed his theory: People who obtained their water from
upstream of the London Thames River water supply had a much lower
incidence of cholera, while those who got their water from the Thames
became sick
nine times more often! Building on this and other
evidence, Snow expanded his earlier writing and re-published it as a
well-researched book in 1855. A decade later, in the 1866 third wave of
cholera, another epidemiologist confirmed Snow's theory, but still the
germ itself hadn't been identified. Indeed, for over twenty years the
conflict between the miasmatists and contagionists continued---with
residues continuing for yet another twenty years, even after the germ
had been found. Honored more posthumously, he is now considered another early pioneer of epidemiology.
|
Nevertheless, Snows findings did not receive a positive reception.
Those in power were torn between the miasmatists and the lawyers
arguing that government had no right to tax private property-owners to
build sewers. Government bureaucrats and members of Parliament were
concerned that sewer systems were
costly. Perhaps they could control the infection by
increasing the quarantine measures. So, like Lister, he and those who
came after him kept accumulating evidence. What was needed was to
identify the causative agent, and this was done two decades later:.
Robert Koch
In the ensuing period of the 1860s and 1870s progress was made in the
field of germ theory, as discussed in the first and second lecture.
Let's move the time up then to 1870s, when Dr. Robert Koch finally was
able to identify the cholera germ. (There are
stories upon stories in all of these, but I’m trying to be selective.)
He, too, was gaining status, as did Pasteur. The germ theory itself was
gaining acceptance, but Pettenkofer didn’t give up that easily. At one
point—here’s another story:
Pettenkofer offered to drink cholera germs. He maintained that the
germs without the accompanying miasma and certain earth-influences
wouldn’t make you sick! And he did! And he didn’t get that sick!
Proof to him. Koch didn’t even acknowledge this. The miasmatists were
losing influence. Finally, Pettenkofer, in spite of many awards and
honors, perhaps he realized he might have been wrong? – he shot
himself. Ah. Because, as I said, his efforts probably did more to
influence the authorities to install water treatment and adequate
sewage than the work of the contagionists. Right for the wrong reasons.
Koch, about whom I spoke three sessions ago in the
lecture 2 on infection,
a pioneer in bacteriology,
continued to gain eminence in the 1880s. He confirmed the bacterium
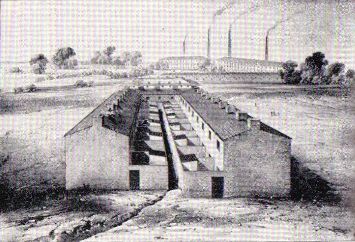
Vibrio comma as the etiologic or causative agent. Hamburg, 1892:
Another wave of cholera. England had begun to install water
purification plants and better sewers, as did many places. In Hamburg,
struck by another epidemic, those in nearby suburb of Altona were
spared. They had installed a water filtration plant. Hamburg’s
governors chose to make that an option reserved to the private owners.
Koch did some site epidemiology and instituted a variety of techniques:
(1) Isolate the cases and destroy chemically their wastes—don’t let
that stuff re-enter the water supply. (2) Disinfect homes so that
residues of diarrhea aren’t picked up by flies. Clean up in general.
And these techniques are seen in the pictures to the right---(near) a
cholera hospital for the Hamburg epidemic; and a special disinfectant
team.
Continuing Efforts
Alas, cholera has a world-wide distribution and won't go away
easily. The map on the left shows where it crops up every once in a
while. Epidemics continue in areas that don't have strong sanitation
infrastructures. Many times during the 19th century the
pilgrimage (haj) to Mecca was disrupted by cholera epidemics.
But people were learning special techniques for working with the disease.
Typhoons (the Pacific name for a hurricaine) lead to flooding, and
fecal material is washed out of cesspools, so cholera is a danger.
(There was danger in Louisiana and Texas in the last few years, but it
didnt't happen.) On the right techniques similar to what Koch suggested
a century ago are being used in cholera epidemics: This in Dakha,
Bangladesh, around 1971:
Another breakthrough is the use of rehydration therapy mentioned above.
Here it is being used for an outbreak of cholera in Peru around 1991.
And of course we have heard about the unfortunate
events more recently in Zimbabwe when government mismanagement leads to
a sanitary infrastructure breakdown----and by that I mean that feces
come to contaminate wells.
Medicine and Public Health.
The
second aphorism of
Hippocrates notes that the doctor should also..."make the externals
cooperate," by which I think is meant that it is fitting for physicians
to participate in advocacy for public policies for the common good. We
must not assume that doctors have much actual power. The short period
of high status in the 1950s was an anomaly, riding on the crest of a
series of major breakthroughs. (Indeed, the doctor's authority was so
esteemed that it was mis-used to sell cigarettes!) Because of the rise
of managed care and third-party payors since the 1970s, though, doctors
have had to struggle to get their message across. This was so in the
first quarter of this century (as noted in the
story of pellagra),
and it is sadly so today, when doctors have been demoted to the
category of providers by the
corporations who run health insurance. Anyone who can receive
payment---chiropractors, massage therapists, nurses---all are also
"providers.").
Hookworm
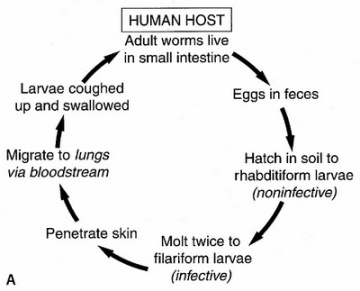
28. Let’s move to another disease of sanitation, Hookworm, which is
prevalent in over a billion people worldwide. It's like cholera
in that it requires a degree of warmth as well as moisture—plus
poor sanitation; but the germs aren't drunk in the water; rather, they
enter as microscopic worm larvae that invade the bare skin of the feet
as you walk on the ground. Although this condition has been around for
probably centuries, but we've only really known about this tiny worm
for a couple of centuries. The American hookworm probably came over
with the slaves. There's also a European and Mediterranean hookworm,
Ancyclostomata, which is only slightly different in some respects, but
its life cycle and dynamics of contagion are the same.
These worms are about a quarter-inch long, narrow, the ones
on the left enlarged about 12 times. They attach to the small and large
intestine, and suck blood.
As for their mouth-parts: Little vampires, they are.
And they embed themselves in the side of the intestines: Here's a microscopic side view of that right below:
 : :
|
There they feed, lay thousands of eggs a day, and co-exist.
Interestingly, there is some evidence that a light infection of
hookworm
actually helps the body to be resilient, and researchers are exploring
the idea of giving selected patients a light dose of hookworm as a
treatment for certain intractible chronic
inflammatory diseases like Crohn’s disease, ulcerative colitis, even
asthma. So far there have been some promising results. (The use of
less-than-disease infection to prevent disease is a recognized
but not widely used method, and another example is the application of
otherwise sterile maggots---fly larvae---to eat any necrotic tissue in
the treatment of bedsores..
By
accident, Arthur Loos in Germany spilled a solution of larvae on his
arm and found he had a skin rash similar to what some folks call ground
itch on their feet. He checked his stool in a few weeks and
there were the eggs. He repeated this experiment, taking thymol to rid
himself of the worms. Thus through serendipity, we benefited from the
unexpected good fortune that Pasteur noted when he said, "Chance favors
the prepared mind." Loos elucidated the life cycle: Hookworm isn't
caused by drinking the feces-contaminated water (as in cholera) but
through the skin, by walking on the ground. Part of this also was
because by the end of the 19th century microscopes of sufficient power
were coming into wider use.
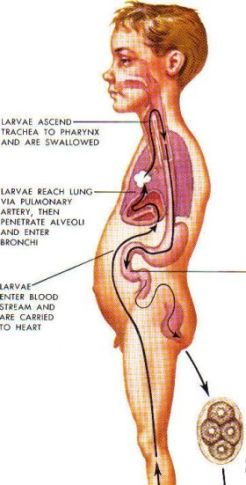
So here's the life cycle:
|

|
|
The eggs hatch into tiny tiny worms, much smaller than the adult size,
small enough to be effectively invisible and also to penetrate the skin
without much effort. (The
skin should be recognized as being a little porous—a sheet of cells
that small critters can burrow through.) Depending on how many times one walks over larvae-infested
moist earth with bare feet or porous or shabby shoes—they can get
through those, too— a person may have a light or heavy infestation..
|
The micro-larvae, tiny roundworms, then penetrates the human skin,
particularly between the toes of bare feet, and is transported through
the capillaries into the venous system
Then, (upper right picture) from
the venous system, the micro-filiarae go into and out the right side
of the heart through the pulmonary artery into the lungs. There the
blood gives off carbon dioxide, picking up oxygen, with the help of the
iron in the hemoglobin molecule. |
Meanwhile, the micro-worm-larva
escapes into the air sacs or alveolae; and gets covered with mucus,
carried up the bronchial tree as phlegm; where it is coughed up and
swallowed, is carrie down into the intestines, burrows into the lining
of the small intestine and matures. Then it cross-fertilizes and can
lay up to 10,000 eggs a day! |
|
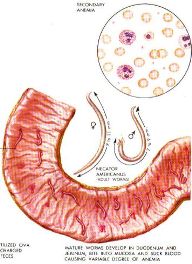
The hookworm causes illness primarily by ingestion of
the host’s blood leading to chronic anemia, and chronic anemia
generates its own secondary features. It’s an iron deficiency anemia,
in part—as I spoke about in last week’s lecture. And there’s a leakage
of serum, and the protein parts of serum. Note the blood cells
portrayed on the left are quite pale---it's called "hypo-chromic,"
meaning low-color, meaning low levels of hemoglobin, due to the chonic
loss of iron. If a person eats a diet rich in iron, this isn't so
pronounced. But the condition is made much worse if there are alos
other types of malnutrition, again described in
last week’s
lecture—such
as pellagra, low-grade scurvy, or other deficiencies. Hookworm was
called “the germ of laziness,” as it became
apparent that the lazy, shiftless "white trash" and negro slave wasn't
in fact lazy so much as genuinely fatigued, and that in turn was due to
severe anemia. That would make anyone seem lazy! Chronic anemia is also
bad for the heart because that organ has to beat harder to try to get
oxygen to the tissues. People with anemia not only feel tired very
quickly, but they also just feel malaise, a general sensation of not
being well.
This seeming laziness and other behaviors when people are sick and
malnourished was alluded to also in the previous century by
Pettenkofer, who advocated nutrition and fresh air, adequate warmth as
well as clean water, and finally was able to sell his program on the
argument that healthy workers are more productive and economically
efficient. (Rockefeller came to a similar conclusion years later, which led to his funding a program for hookworm eradication.

|
The hero for the story of the recognition and treatment of hookworm in
America is Charles Wardell Stiles, a parasitologist (a kind of
zoologist) who studied in
various places in Europe as so many late 19th century scholars
did—America being relatively intellectually impoverished, especially
scientifically, in that era. He learned about hookworm, and became
aware that it was common in the South. Probably it was a major cause of
death at the infamous Andersonville confederate prison for
captured union troops, who died in the thousands from disease. Most doctors didn’t recognize the prevalence of this disease,
attributing the symptoms to sheer laziness and lack of character. They
were shocked to find how widespread and common it was!
There’s a whole sub-story here about how Stiles and a few other
people finally maneuvered and sold the public health approach, and John
D. Rockefeller Junior (shown at left, picture taken around 1910), who at that point had inherited his father’s
wealth (near left they are walking together) seeded a health institute and invested in a program to educate
folks. This was partly altruistic and partly economic good
sense—healthier workers make for more prosperity.
Another pioneer in the field of hookworm research was Dr. Charles C.
Bass, (shown to the right), of the Tulane University School of Medicine
in New Orleans. Later in life he became a pioneer of plaque control in
dental hygiene (about which we'll talk later in this lecture, and this
also has its own webpage). Bass co-wrote one of the first books on the
nature of hookworm disease---life cycle, diagnosis, treatment,
prevention.
The Anti-Hookworm Campaign in the South (1910-1915)
The key was a mixture of things: First, there was treatment,
which
was uncomfortable, involving a chemical that killed the worms, or at
least stunned them and made them loosen their grip, and then a strong
purgative, generally Epsom salts, to wash it out. But that wasn’t
enough. How to prevent re-infection? A variety of chemicals were
used over the next twenty years, with fewer side effects. Some of the
improvements were dramatic, people becoming far more active, feeling
better. (There's a humorous story of one uneducated fellow
complaining in a letter that, in feeling better, he also became more
physically
aggressive and got into trouble for that!)
The plan was to generate a new social norm. (This could be
an interesting social studies project for high school students! How
would they plan such a promotional- educational program?) In the south,
the planning drew a bit on the ritual of the religious revivals, making
it a social affair, with food, speeches, honoring guests.
Another technique was the use of handbills, announcements: as at right.
The problem is that sanitation takes work, and if you have no
energy, and feel bad, there’s little motivation to keep a clean home.
Also, building a proper privy took time, required supplies, was a
hassle. Also, they attracted flies, unless screening was easily
available, and stunk—the bushes were cleaner.
But people couldn’t afford shoes; and shoes in those years often didn’t fit well and hurt!
Even less could you afford shoes for kids who then grew out of them too quickly!
Still, the Rockefeller-funded campaign was promoted—there
were a number of heroes here, as it was multi-state, regional, and in
the face of a wide range of resistances. Set it up at the fair, make it
the in-thing to do.
The same problem is going on today, by the
way, in rural China, india, and elsewhere: It's quite a challenge to sell people on effective fecal waste
control!
Part of the problem is that it is easy to do it wrong, to not
have the proper equipment. For example, on the right, if one builds the
cesspool under
the privy so that it is really just a gap in the rocks, it's likely to
leak the contents downward into the creek, which pollutes all those who
live downstream.
The WPA in the Depression advanced this significantly—playing off
George Murray’s presentation on the Depression and what was done. I
want to say that even today there’s a question as to how to spend the
money, and the investment in infrastructure versus just loans so
someone can borrow to open a little boutique— community versus private
enterprise– is a lively balance. And let’s not forget sewage and water
treatment—as a book on toilets and waste control points out, we need to
address this problem even today in the USA!
Children’s health-promotion books are still being written and used today.
Below right is a promotional signs for proper privy building, setting.
So there have been continued efforts in this direction. The
international work continues to be challenging, and the Bill and
Melinda Gates Foundation recently gave a multi-million dollar grant to
the Sabin Foundation to do research on a vaccine against hookworm.
The real moral of this story is that public health has to not just sell
to the bureaucrats and politicians, but also to the people, when a
change of personal health habits are needed. (Of course this has
relevance today in considering the major challenges of smoking, alcohol
abuse, drug abuse, lack of exercise, obesity, unsafe sex, premature or
unwanted pregancy, reckless driving or driving without seatbelts, and
other public health challenges. We are all being asked to subsidize
these follies through higher taxes and medical insurance premiums, and
we no longer can afford to do so.)
Dental Hygiene & Plaque Control
The last third of this lecture is devoted to another problem in
hygiene---dental hygiene. It's not just about brushing your teeth and
avoiding sweets---that we learned about in school. Since that time,
though, the microbiology and biochemistry of dental plaque---that
build-up of bacteria and secretions at the gum line---has been
implicated as the major cause of tooth decay, and I discuss that with
pictures more fully
on an associated webpage. (It may also affect other health problems, too!)
Summary
This webpage presents the lecture I gave on March 2, 2009, for
Senior University Georgetown. I described some stories regarding the
discovery of the cause of cholera,
especially in the 19th and 20t century; stories about the disease
of hookworm, especially in the early 20th century; and in that
talk and a
related webpage,
the rationale for the use of
dental floss in preventive dentistry. All three endeavors are ongoing.
Cholera is still present with epidemic outbreaks wherever water
treatment is not optimal. Hookworm is still prevalent where people walk
barefoot and defecate onto the ground---which still happens in many
parts of the world. And middle-aged people are still losing teeth
unnecessarily because of gum disease and cavities that could be
prevented by flossing regularly; and many people in our own culture
still hardly appreciate exactly why they should develop this hygiene
habit. As I said, I found that the history of medicine demonstrates how
we can be wrong and also right, or vice versa, as we collectively grope
towards more useful understandings of our world and seek to promote
healing. In studying for and making these presentations, I confess that
I realized more fully how in a larger sense this is also for me a
spiritual path. I invite you to read
these stories and the other lectures on the website, and tell friends
about them. We can learn from
stories—not just Bible stories, but all sorts of stories. History can
be a great source of various kinds of lessons. I hope you have enjoyed.
References
Altman, L. K. (1987).
Who goes first? The story of self-experimentation in medicine. New York: Random House. [pp. 23-25 on Pettenkofer; pp 166-169 on Arthur Loos.]
Bray, R. S. (2000).
Armies of pestilence: the impact of disease on history. New York: Barnes & Noble. (Chapters 19-22 on Cholera.)
Franklin, J. & Sutherland, J. (1984). Max von Pettenkofer: The last of the miasmatists (ppg 139-182), in:
Guinea-pig doctors: self-experimentation in medicine. New York: William Morrow & Co.
Magner, Lois N. 1992.
A history of medicine. New York: Marcel Dekker.
Magner, Lois N. 1994.
A history of the life sciences (2nd ed.). New York: Marcel Dekker.
Williams, Greer. (1969).
The plague killers. New York: Charles Scribner's Sons.
: